Guest Post by
Sam Winter, Ph.D.
Faculty of Education,
University of Hong Kong.
Previously a member of the
World Health Organization (WHO)
Working Group on Sexual Disorders and Sexual Health.
[Formatted pdf version of this paper]
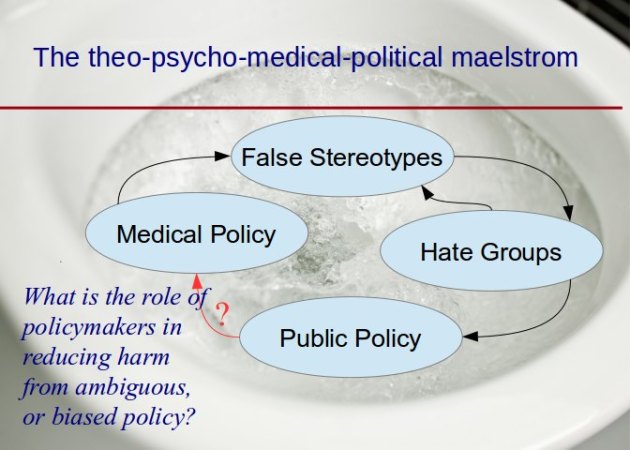
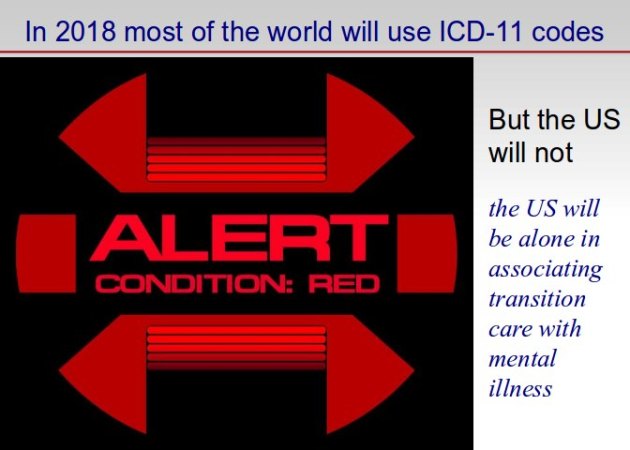
As most visitors to the GIDReform Advocates site will know, the World Health Organization (WHO) diagnostic manual (commonly known as the International Classification of Diseases) is currently under revision. The new edition, ICD-11, is slated for approval in 2017. I was a member of the WHO Working Group on Sexual Disorders and Sexual Health (WGSDSH), the eleven-member group which proposed a number of revisions relevant to trans people. The original WHO plans, for all our proposals to be loaded in October 2012 onto a website, for all the world to see (and comment on), never happened. Indeed, the WHO Secretariat running the show have imposed, apparently as it suits them and somewhat inconsistently, fairly onerous confidentiality rules which have prevented WGSDSH members and others from openly sharing what is going on. That said, WHO has shown itself to be comfortable with releasing material from time to time, particularly at academic conferences, as well as in the odd journal article.
One such article, in late 2012, was the one by Jack Drescher, Peggy Cohen-Kettenis and myself (all of us WGSDSH members) in which we reported a key proposal, that current ICD diagnoses commonly used with trans people (the flagship diagnosis for adolescents and adults being transsexualism) should be replaced by one called gender incongruence, and that this diagnosis should be moved out of ICD’s Chapter 5 (Mental and Behavioural Disorders) and into another chapter. Our rationale was that it was important to retain access to gender affirming healthcare for those trans people who needed it, but that the classification as a mental disorder actually undermined that goal, as well as adding to stigma. Our preference was for placement in a stand-alone chapter, but (with this prospect unlikely) an alternative was placement in a broad chapter on sexual and gender-related health.
In a corner of a little table within that article we were able to mention that the proposal was actually for two gender incongruence diagnoses: Gender Incongruence of Adults and Adolescents (GIAA), and Gender Incongruence of Childhood, for children below the age of puberty (GIC).
The appointment to the WGSDSH was for two years. The two years is well and truly over. It has been a long time since WHO Geneva wrote to me about anything. I do not know whether the WGSDSH still exists. If it does I assume I am no longer a member. So now I can talk.
The GIC proposal has been hatched in a small WGSDSH sub-group consisting of three members (in which my voice was a minority). It was never properly discussed in the full WGSDSH. I had misgivings about the proposal. The case for a diagnosis, to be used with gender different children below the age of puberty, seemed uncertain. My misgivings grew as a result of discussions with trans activists. They continued to grow as reports came in from independent reviewers contracted by WHO to look over the WGSDSH proposals. My attempts to have the GIC proposal discussed in the full WGSDSH were stifled by the WHO Secretariat. It became clear to me that WHO was committed to going ahead with the GIC proposal, at least as far as field trials, and that I would have to work against this proposal from the outside.
The arguments for GIC (commonly that it is needed to justify the existence of specialist clinics, for training purposes, to generate research) really don’t stand up to scrutiny. Worse, the GIC case was entirely undermined by the fact that we (WGSDSH and WHO) were making entirely different proposals in regard to young people exploring (and learning to become comfortable expressing) their sexual orientation. The proposal was that disease diagnoses for these individuals should be removed. And yet here we were, proposing a disease diagnosis for young children exploring (and learning to become comfortable expressing) their gender identity. It seemed to me that there was a hypocrisy at play, and a transphobic hypocrisy at that.
Finally, with Cochran et al’s new paper in the WHO Bulletin which makes public for the first time the proposals for the sexual orientation diagnoses, I am able to release a report I wrote last year, first of all for the WPATH ICD Consensus Meeting in San Francisco (the one that split 14:14 on the GIC proposal) and then for the Global Action for Trans* Equality (GATE) Experts’ Meeting in Buenos Aires (the one that produced alternative proposals for meeting the needs of gender different children).
The opposition to the GIC proposal has now become a worldwide chorus. As well as the voices of GATE, and voices within WPATH, there is the International Campaign Stop Trans Pathologisation (STP), which recently focused its campaign on fighting the pathologisation of children. Participants at a recent trans health conference in South Africa are developing a Cape Town Declaration calling on WHO to discard the proposal. Several other community and professional groups are discussing the issue and can be expected to voice their opposition in the future.
In order to facilitate the debate, I offer here on GIDReform a reduced version of the paper I wrote for the earlier two meetings (WPATH Consensus and GATE Experts’). Some of you may have read it as an Appendix to the WPATH ICD Meeting Report (pages 58-67).This paper makes reference to other documents available to participants at the WPATH Consensus Meeting, but not included here. Readers can access some of those documents, cited in the report of that meeting.
Arguments against the proposed Gender Incongruence in Childhood diagnosis.
In this document I present arguments against the draft proposal for a diagnosis of gender incongruence in childhood (‘GIC’).
Briefly, I believe that the proposed GIC diagnosis pathologises patterns of development that should not be pathologised, that the diagnosis is inconsistent with the approach the Working Group proposes for other children and youth (including, importantly, homosexual youth), that the pathologisation carries risks for the gender-different child (and indeed for the broader work of the Working Group), and that there are alternative ways of providing health care services for gender-different children (plus their parents, teachers and others) who may need such services.
In short the argument is for de-pathologising, rather than simply de-psychopathologising, gender difference in childhood.
A few words about my role in this process. I am the member of the WGSDSH1 (the ‘Working Group’) which has worked on developing the draft proposals you have in your papers. I was also in the small subgroup which worked on the draft gender incongruence proposals, again in your papers. With the other two members of that subgroup I am a co-author of the Minding the Body paper,2 which argues for removal of transgender diagnoses from ICD Chapter 5 (Mental and Behavioural Disorders), and which has, in the table on p570, drawn wide attention to a proposed child diagnosis.
I, like others, have misgivings about the GIC proposal; a proposal which focuses on gender incongruent children below the age of puberty. My concerns have grown in recent months, largely as a result of discussions with professionals and scholars working in the field. Letters from the following persons not at the meeting have been made available to participants at this meeting: Dr Elizabeth Riley (counseling psychologist working in Sydney, Australia), Dr Lisa Griffin (clinical psychologist, working in Virginia, USA), Dr Antonia Caretto (clinical psychologist, Michigan, USA), Dr Kelley Winters (author of the book Gender madness in American psychiatry, currently resident in Florida USA), and Dr Arnaud de Villiers, medical clinician and activist on transgender health issues in Africa (Cape Town, South Africa). They all express some sort of misgiving about the child diagnosis, and many argue the sort of strategies I argue for here. Indeed my ideas have in some cases been shaped by their own.
Please note that my own misgivings place me in a minority (of one) in the small subgroup which has worked on the Working Group gender incongruence diagnoses. As you might expect, I am therefore not a co-author of the Background Discussion Document3 (provided by WHO and among your papers), recently prepared (I assume) by the other two subgroup members.
I am comfortable sharing my perspective on the proposed GIC diagnosis. My contribution to this debate is my acquaintance with the broader aspects of health and rights for transgender people, particularly as those things apply in Asia.
Here are my arguments in more detail.4
_________________________________________
1: The view of gender-different children as sick and in need of health care is a culturally-specific one, not only modern but also peculiarly Western in origin.
It is clear that many transgender people worldwide5 live in cultures that are more accepting of gender difference than is the case in much of the West. Many of these cultures have a long history of inclusivity in regard to such persons,6 inclusivity that was anathema to European colonists and missionaries,7 but some of which survives to this day.8 In these cultures there are often a range of identities available to young children who grow up gender-different.9 Many of these roles had (or indeed still have) particular social, cultural, or even spiritual or religious significance.10 Today, in parts of the global south and east, many such children begin to identify in another gender quite early in life, doing so before puberty, and are recognized by others as being members of their affirmed gender group, even if in the modern world there are often, at home and school, limits to the degree to which they can express that identity. Those limits in any case often loosen by the time they approach school-leaving age.
Many individuals growing up in these social environments appear to enjoy (in childhood, adolescence and adulthood) relatively good psychological adjustment (despite sometimes having to endure broader societal stigma).11 Though a gender-different child’s gender identity and expression may not be universally celebrated by parents and teachers, that identity and expression tends to be accepted by them as diversity rather than mental or medical disorder. In thirteen years working in with transgender people in Asia I recall very few informing me that their parents had taken them to see a doctor when they were a child. Asian transgender activists who have written to me since my arrival in San Francisco a couple days ago confirm that it is relatively rare for parents to do so.
The view of gender-different children as sick is therefore a somewhat culture-specific one; not only modern but also peculiarly Western. (And it is a view that may aggravate whatever societal stigma is out there, but I’ll come back to that point later).
Now let’s consider what health care we actually provide to these ‘sick’ children (those who according to this Working Group proposal would be diagnosed as gender incongruent).
2: Gender-different children have no need of hormones or surgery, or any other somatic gender health care. Insofar as they may benefit from any health care services at all (and an indeterminate number may not need it) their needs are focused on accessing counseling and (perhaps) other mental health care.
They may need support and information to help in exploration of their gender issues (for example ‘Who am I?’, ‘What shall I do about it?’), ways of dealing with the challenges arising from gender expression (for example ‘Why won’t people let me be who I want?’, ‘Why do they treat me the way they do?’, ‘How should I handle this?’) and arising from any bodily concerns they may have (for example ‘Why do I feel this way about my body?’, ‘What can I do about it?’, ‘When?’, ‘With what effects?’). Parents, teachers and siblings may also benefit from some support information about gender issues, and from counseling as to how they should respond to their child’s gender issues.
I suggest all this provides no justification for a transgender specific and pathologising diagnosis of the sort the GIC represents. Consider, for comparison, other children with identity issues, or who find themselves confronted by circumstances (either in or out of their control) which bring them pain. An ethnic minority boy may want to explore his ethnic identity, and deal with the difficult or painful challenges of living in a racist society. But we do not diagnose him as having an ethnic disorder. A girl with divorced parents may need to explore difficult or painful family issues, and deal with unkind teasing at school. But we do not diagnose her as having a divorce disorder. A girl and her parents may want her to be top in the class, and she may feel great pain for not achieving this, and experience rejection at home. But we do not give her a diagnosis of educational aspiration disorder. In all these cases the child needs (and a health care provider would hopefully seek to provide) information, support and a more supportive environment that enables the child’s development. But he or she would do this without pathologising the child who finds him/herself in this situation. It is difficult to see why it should be different for gender-different children.
What about those relatively few gender-different children who actually experience clinically significant distress about their situation. They may feel suicidal. They may be on the verge of self harm. For them there are already diagnoses available, the same diagnoses that might be used with a child clinically depressed or anxious in regard to ethnic minority status, parental separation or inadequate achievement. Of course, one would want to ensure that such diagnoses are not used to justify gender reparative care. But this is where Z codes can come in (more on this later)
One does not have to think of the ethnic minority child, the child from a broken family or the child with unmet achievement goals to see an inconsistency in the way the needs of the gender-different child are addressed. A comparison is even closer to home – gay and lesbian youth. And that leads us to the next section.
3: There is a grave inconsistency in the way the Working Group proposes to address the health care needs of (on one hand) gay and lesbian youth and (on the other) gender-different children.
The WHO Working Group has recommended deletion of the entire F66 block (‘psychological and behavioural disorders associated with sexual development and orientation’). Used with youth, F66.0 (sexual maturation disorder) currently pathologises the teenager who is distressed about his uncertain sexual orientation. F66.1 (ego-dystonic sexual orientation) currently pathologises the teenager who, knowing his or her sexual orientation, wishes it were different. The first youth needs support in exploring his or her sexual identity, and the second youth needs help in coming to terms with it, learning to feel comfortable expressing it, and dealing with the stigma and prejudice that comes from expressing it. These are needs that are directly analogous to those of gender-different children.
F66.0 and F66.1 (and a third diagnosis, F66.2 (sexual relationship disorder)) are widely regarded as providing a final repository for the thinking that underpinned the old homosexuality diagnosis (after all, how many youth are distressed by the possibility they may eventually turn out heterosexual, or about the actual fact that they are?). Part of the concern over the F66 block is that it raises possibilities for psychopathologising sexual variation, and for prompting or justifying stigma and human rights abuses, including sexual reparative therapy.
Few reputable clinicians would disagree with the proposed deletion of Block F66, or with the proposal that those with sexual orientation issues who would genuinely benefit from mental health care could be provided access to it by other diagnostic means. Significantly, the Working Group proposes that Z Codes may be used in these cases.
The F66 proposals present a gravely inconsistent approach. The inconsistency is in the way we address the mental health care needs of (on one hand) the gay and lesbian teenager exploring and coming to terms with his or her sexual orientation (and the expression thereof) and (on the other) the gender-different child exploring and coming to terms with his or her gender identity (and expression thereof). For lesbian and gay youth the move is away from diagnosis that pathologises. For gender-different children the Working Group proposes that a pathologising approach continues.
This inconsistency is all the more perplexing in view of the fact that, despite their names, the current sexual maturation disorder and ego-dystonic sexual orientation diagnoses (both proposed for removal) both explicitly incorporate gender identity.12
4: There are important implications for the prospects of removing the proposed gender incongruence diagnoses from Chapter 5.
The GIC diagnosis, a transgender specific diagnosis affording access only to mental health care, may conceivably come at the price of failure in broader moves to remove both diagnoses (GIC and GIAA13) from Chapter 5. Let me explain why I think this.
a. Undermining the case for removal of GIC from Chapter 5. A recommendation for a GIC diagnosis – a diagnosis aimed to facilitate health care that is exclusively mental health care – is fundamentally inconsistent with a recommendation to remove that diagnosis from Chapter 5 (the mental and behavioural disorders chapter). Indeed, with mental health care the only sort of help to be provided to the child, Chapter 5 would appear to be an obvious place for the diagnosis. The case for de-psychopathologisation of childhood gender difference is therefore undermined, and the case for retaining the child diagnosis in Chapter 5 is inevitably left in place for all those who would use it. This carries risks for ( a ) reduced recognition of gender status (e.g. the little transgender girl seen as a mentally disordered boy), ( b ) increased stigma, and ( c ) increased use of gender reparative approaches.
With regard to gender reparative approaches, the removal of F66.0 and F66.1 (diagnoses that have been used, for example in Hong Kong, to justify sexual reparative therapy) may increase the risk that some mental health care providers will resort to child gender reparative approaches, rationalised in terms of attempting to catch incipient homosexuality early and nip it in the bud. I suggest that this risk would be even higher if the proposal to remove the GIC diagnosis from Chapter 5 were to be rejected.14
b. Undermining the case for removal of GIAA. In view of the sibling relationship between GIC and GIAA (a relationship which is noted in the GIC Background Discussion Document) the case for removing the latter from Chapter 5 may also be undermined. The prospect that both diagnoses might stay in Chapter 5 is as alarming for transgender people in the global south and east as it would be for transgender people elsewhere. The idea that transgender people are mentally disordered already has a foothold there, and it appears to contribute to the stigma that sometimes blights transgender people’s lives. A recent research study in five Asian countries, as well as in the UK and USA, indicates that in Asia, as elsewhere, people who believe that transgender people suffer from a mental disorder also tend to harbour prejudiced attitudes towards them– attitudes which, if expressed in discriminatory behavior, would act to push transgender people towards the margins of society (Winter et al, 2009).
Those working in the West (or in countries influenced by the modern Western discourse on psychopathologisation) may sometimes forget that support for removal of the trans diagnoses from Chapter 5 is less than universal; there are plenty of clinicians worldwide who take a different view. Significantly, dissent was evident even among the experts WHO recently invited to review the Working Group proposals. One, from a place other than North America or Western Europe, remarked on the longstanding and broad consensus among health experts in his country that gender incongruence conditions are mental disorders, disorders that obviously involved a distortion of mental processes contributing to the formation of sexual identity.
In May 2015, the World Health Assembly, the governing body of WHO, is due to vote on ICD-11. Some proposals will no doubt prove more contentious than others. Insofar as there are clinicians and scholars internationally who share the views of the above reviewer, and (either as individuals or through their professional associations) have the ear of their governments, there is a risk that the proposal to remove GIC (and by extension GIAA) from Chapter 5 will be undermined.
_________________________________________
With so many problems plaguing the GIC diagnosis, what is the way forward? The rest of this paper presents ideas. They are the product of long discussions (face to face and by e mail, with clinicians, scholars and activists worldwide.
A way forward.
An important way forward is provided by the non-pathologising Z codes.15 As is evident from the introductory material in the Z-Code chapter, these codes are designed for circumstances matching those in which gender-different children are liable to find themselves. 16
Importantly, the Working Group document which provides a rationale for deleting the F66 proposals notes that Z codes are an alternative (and less pathologising) way of providing health care to those with sexual orientation issues who are currently at risk of receiving a F66 diagnoses. Particularly relevant here is a section entitled ‘What is a disorder vs. a perceived need for mental health services?’ I quote:
……the ICD is structured to allow for two possibilities. First, the individual might have a clinically recognizable set of set of symptoms related to particular life circumstances, such as relationship distress, that is not a mental disorder, but it co-occurs with a recognizable mental disorder, such as Major Depression. In this situation, the diagnosis of Major Depression is applied. In the second situation, the individual may have a clinically recognizable set of symptoms, or ’problems’ but no underlying disorder. In this case, a Z category may be selected. The Z categories recognize that individuals can and do seek services, including mental health services, in the absence of a current mental health or behavioural disorder. For example, requesting help for tobacco cessation in the absence of tobacco dependency (Z72.0), or for assistance in developing coping skills when targeted for discrimination (Z62.5) are both types of presenting concerns that could result in classification with a Z category. A health encounter in which the person is requesting information about sexual matters in the absence of a mental disorder could be classified using a Z category as well. In this way, the ICD distinguishes between mental disorders and perceived need for mental health services in the absence of a diagnosable disorder.17
The Working Group then goes on to make three recommendations, as follows:
a) The deletion of the F66 categories in their entirety: As the review above demonstrates, the F66 categories do not meet the requirements for retention in the ICD-11. There is no evidence that they improve clinical utility, and reason to believe they create harm; no evidence of public health surveillance need; no evidence of research needs in order to track mental health morbidity; and the categories themselves raise significant human rights concerns.
b) The revision of several of the Z70 categories to better address sexual health and sexual relationship concerns at a more general level. These changes would focus more clearly on common reasons for seeking services as well as remove unnecessary focus on sexual orientation that currently lacks justification.
c) The revision of the descriptions of the Z60.4 and Z60.5 categories to encompass sexual orientation concerns. These changes would facilitate accurate coding of personal distress resulting from experiences with anti-gay stigma, and may also be useful as a part of public health surveillance to track human rights concerns related to sexual orientation. 18
A similar approach can be taken with those children liable, under current proposals, to be diagnosed with the pathologising GIC category. There are a number of Z codes that could prove relevant to the needs of gender-different children, to document examinations and other health encounters.
At the WPATH Consensus Meeting I presented proposals for ways in which the Z Codes could be used to facilitate appropriate health care for those gender-different children who might benefit from it, as well as to document contact with health care services. I argued that these codes could be used to help children explore and express their gender identities (and to support their efforts to cope with stigma) in the same way that the Working Group is proposing that the Z Codes could be used with gay and lesbian youth exploring and expressing their sexual orientation (and, again, to support their efforts to cope with stigma).
A more detailed proposal for using ICD-11 Z Codes to facilitate access to support services for trans and gender different children was developed at the GATE (Global Action for Trans* Equality) Consensus Meeting in Buenos Aires, April 2013.1920 It recommended revisions to include gender identity, gender expression as well as sexual orientation in codes:
Z60.4- “Exclusion and rejection on the basis of personal characteristics…”
Z60.5- “Persecution or discrimination, perceived or real, on the
basis of membership of some group…”
Z70.4- “Counseling for a child to support gender identity or
expression that differ from birth assignment.”
Z70.2x- “Counseling for families and service providers related to
gender identity or expression of a child.”
Importantly, where a child is genuinely suffering from anxiety and mood disorders associated with gender difference, Z Codes can be used to specify the nature of the distress, thereby enabling appropriate health care for the child involved. Further, when a child reaches puberty and is in need of puberty blockers (where they are available), Z Codes can be used to document a history of gender difference, thereby ensuring a prompt diagnosis of GIAA.21 Finally, when a gender-different child seeks adaptation at school (or elsewhere) to accommodate his or her gender difference, Z Codes can be used to provide a basis for the case being made.
In short, it is clear to me that Z Codes can play an important and appropriate role in provision of health care for gender-different children in their pre-puberty years, covering a wide range of encounters with health care providers, and a variety of health care-related services appropriate to their needs.
It is to be hoped that a Z Code approach with gender-different children will make it more likely that such children do indeed grow up comfortable with their gender; in the words of Jazz, liking who they are.
Footnotes:
1 The WHO Working Group on Sexual Health and Sexual Disorders
2 Drescher, Cohen-Kettenis and Winter (2012)
3 Background Discussion Document on Proposed ICD-11 Category of Gender Incongruence of Childhood.
4 Childhood gender diagnoses have been the subject of much criticism. The Background Discussion Document on GIC to which I referred earlier reviewed some of the published critiques in the area, most of them in relation to the old DSM-IV diagnosis, gender identity disorder of childhood. I will not revisit that research here. I will add though, that the above document neglects to mention publications by experienced clinicians advocating gender affirmative approaches in work with these children and critical of less affirmative (and even repressive) approaches (Ehrensaft, 2011). Other recent additions to the literature are three Australian papers examining the views of three groups of stakeholder (parents of gender-different children, professionals, and transgender adults) on the needs of needs of gender-different children and their parents. Together they indicate concurrence on the importance of freedom of expression, acceptance, respect and support for the children, and for information and support for the parents (Riley et al, 2011a,b, 2012).
5 In the Asia-Pacific alone there are an estimated 9 to 9.5 million (UNDP 2012).
6 See for example Coleman et al (1992) and Urbani (2006) in relation to Myanmar; Matzner (2001) discussing Hawai’i; Schmidt (2001) discussing Samoa; Graham (2001, 2002) and Graham-Davies (2007) discussing Sulawesi in Indonesia; Jackson (2003) discussing Thailand; and Nanda (2000a,b,c) discussing Thailand, the Philippines, India and across Polynesia. Also see Peletz (2006, 2009) for a more general discussion of cultures of ‘gender pluralism’ in pre-modern Southeast Asia.
7 See for example Nanda (1990, 2000a), Brewer (1998, 2001).
8 For example Graham-Davies (2007); Vasey and Bartlett (2007).
9 For a (non-exhaustive) list of around 50 identity labels used in the Asia-Pacific by and/or for (those we in the West would call) transgender women see UNDP (2012)
10 A recent WHO Asia-Pacific regional consultation on transgender health, having drawn up a working definition of transgender, was at pains to add in an explanatory note: “Transgender persons in Asia and the Pacific often identify themselves in ways that are locally, socially, culturally, religiously, or spiritually defined.” (WHO 2013, page 18, current author’s emphasis).
11 I should stress that gender-different children in the global south and east don’t always find acceptance at home and school; not even in the most inclusive societies. Nor does it mean broader societal acceptance when the child reaches adulthood. The very real difficulties facing transgender people across the Asia-Pacific, particularly in the least inclusive societies, are very well documented. For a review of much of the research see UNDP (2012).
12 So does sexual relationship disorder, though in this case children with gender identity issues are not included.
13 Gender incongruence of adolescence and adulthood.
14 WPATH deems gender reparative approaches with children as unethical. “Treatment aimed at trying to change a person’s gender identity and expression to become more congruent with sex assigned at birth has been attempted in the past without success [references supplied], particularly in the long term [references supplied]. Such treatment is no longer considered ethical.” (WPATH, 2011, p16).
15 Z00-Z13 Persons encountering health services for examination and investigation; Z20-Z29 Persons with potential health hazards related to communicable diseases; Z30-Z39 Persons encountering health services in circumstances related to reproduction; Z40-Z54 Persons encountering health services for specific procedures and health care; Z55-Z65 Persons with potential health hazards related to socioeconomic and psychosocial circumstances; Z70-Z76 Persons encountering health services in other circumstances; Z80-Z99 Persons with potential health hazards related to family and personal history and certain conditions influencing health status.
16 Categories Z00-Z99 are provided for occasions when circumstances other than a disease, injury or external cause classifiable to categories A00-Y89 are recorded as “diagnoses” or “problems”. This can arise in two main ways:When a person who may or may not be sick encounters the health services for some specific purpose, such as to receive limited care or service for a current condition, to donate an organ or tissue, to receive prophylactic vaccination or to discuss a problem which is in itself not a disease or injury.
When some circumstance or problem is present which influences the person’s health status but is not in itself a current illness or injury. Such factors may be elicited during population surveys, when the person may or may not be currently sick, or be recorded as an additional factor to be borne in mind when the person is receiving care for some illness or injury.
ICD-10 online, at http://apps.who.int/classifications/icd10/browse/2010/en#/XXI
17 Rationale for the Deletion of the F66 Categories in the ICD-11, p3.
18 Ibid. p21.
19 Global Action for Trans* Equality (2013) “Critique and Alternative Proposal to the ‘Gender Incongruence of Childhood’ Category in ICD-11,” GATE Civil Society Expert Working Group, Buenos Aires, April 4. http://globaltransaction.files.wordpress.com/2012/03/critique-and-alternative-proposal-to-the-_gender-incongruence-of-childhood_-category-in-icd-11.pdf
20 Winters, K. (2013) “From Gender Madness to Gender Wellness in the ICD-11,” National Transgender Health Summit, Oakland, CA, May. http://www.slideshare.net/kelleywinters/201305-nth-sb
21 Gender incongruence of adolescence and adulthood.
Reference list:
Brewer, C. (1998). Baylan, asog, transvestism, and sodomy: gender, sexuality and the sacred in early colonial Philippines. Intersections: Gender, History and Culture in the Asian Context. Retrieved 15th March 201 from intersections.anu.edu.au/issue2/carolyn2.html.
Brewer, C. (2001). Holy confrontation: religion, gender and sexuality in the Philippines, 1521-1685. Manila: Institute of Women’s Studies, St. Scholastica’s College.
Coleman, E., Colgan, P., & Gooren, L. (1992). Male cross-gender behavior in Myanmar (Burma): A description of the acault. Archives of Sexual Behavior, 21, 3, 313-321.
Drescher,J., Cohen-Kettenis,P. and Winter,S. (2012) Minding the Body. International Review of Psychiatry, December 2012; 24(6): 568–577
Ehrensaft,D. (2011) Gender born, gender made, raising healthy gender non-conforming children. New York: The Experiment Publishing.
Global Action for Trans* Equality (2013) “Critique and Alternative Proposal to the ‘Gender Incongruence of Childhood’ Category in ICD-11,” GATE Civil Society Expert Working Group, Buenos Aires, April 4. http://globaltransaction.files.wordpress.com/2012/03/critique-and-alternative-proposal-to-the-_gender-incongruence-of-childhood_-category-in-icd-11.pdf
Graham, S. (2001). Negotiating gender: ‘Calalai’ in Bugis society. Intersections: Gender, History and Culture in the Asian Context, 6.
Graham, S. (2002). Priests and gender in South Sulawesi, Indonesia Retrieved 14th August, 2011, from http:// web.hku.hk/~sjwinter/TransgenderASIA/paper_priests_and_gender.htm.
Graham-Davies, S. (2007). Challenging gender norms: five genders among Bugis in Indonesia. Belmont: Thomas Wadsworth.
Jackson, P. (2003). Performative genders, perverse desires: a bio history of Thailand’s same-sex and transgender cultures. Intersections: Gender, History and Culture in the Asian Context, 9.Retrieved 30th March 2012 from intersections.anu.edu.au/issue9/jackson.html
Matzner, A. (2001). ‘O au no keia’: voices from Hawaii’s Mahu and transgender communities. Bloomington: Xlibris.
Nanda, S. (1990). Neither man nor woman: the Hijras of India. Belmont, California,
Nanda, S. (2000a). Hijra and Sadhin: neither man nor woman in India. In Nanda, S. (Ed.), Gender diversity: cross- cultural variations. Long Grove, Illinois: Waveland Press.
Nanda, S. (2000b). Transgendered males in Thailand and the Philippines. In Nanda, S. (Ed.), Gender diversity: cross-cultural variations. Long Grove, Illinois: Waveland Press.
Nanda, S. (2000c). Liminal gender roles in Polynesia. In Nanda, S. (Ed.) Gender Diversity: Cross-Cultural Variations. Prospect Heights: Waveland Press.
Peletz, M. G. (2006). Transgenderism and gender pluralism in Southeast Asia since early modern times. Current Anthropology, 47, 2, 309-340.
Peletz, M. G. (2009). Gender pluralism: southeast Asia since early modern times. New York: Routledge.
Riley, E., Gomathi, S., Clemson, L and Diamond D (2011a). The needs of gender-variant children and their parents according to health professionals. International Journal of Transgenderism, 13:54–63, 2011
Riley, E., Gomathi, S., Clemson, L and Diamond D (2011b). The needs of gender variant children and their parents: a parent survey. International Journal of Sexual Health, 23:181–195, 2011
Riley,E., Clemson,L, Sithathan, G. and Diamond,M. (2012). Surviving a gender variant childhood: the views of transgender adults on the needs of gender variant children and their parents. Journal of Sex & Marital Therapy, 00:1–22, 2012
Schmidt, J. (2001). Redefining fa’afafine: Western discourses and the construction of transgenderism in Samoa. Intersections: Gender, History and Culture in the Asian Context, 6. Retrieved March 30th 2012 from intersections. anu.edu.au/issue6/schmidt.html.
UNDP (2012).: Lost in Transition: Transgender People, Rights and HIV Vulnerability in the Asia-Pacific Region. Bangkok: UNDP Asia-Pacific Office.
Urbani, E.R. (2006). Because Buddha was a man: the ambiguousness of spirit mediums in Mandalay. Amsterdam, Netherlands: MA Thesis, Department of Sociology and Anthropology, University of Amsterdam.
Vasey, P. L., & Bartlett, N. H. (2007). What can the Samoan “fa’afafine” teach us about the western concept of gender identity disorder in childhood? Perspectives in Biology and Medicine, 50, 4, 481-490.
WHO (2009), International statistical classification of diseases and related health problems. – 10th revision, 2008 edition. Geneva: WHO
WHO (2013) Consultation on HIV, STI and
other Health Needs of Transgender People in Asia and the Pacific. Report of meeting 11-13 September 2012. Manila: WHO Regional Office for the Western Pacific.
Winters, K. (2008). Gender Madness in American Psychiatry: Essays from the struggle for Dignity, GID Reform Advocates, www.gendermadness.com
Winters, K. (2013) “From Gender Madness to Gender Wellness in the ICD-11,” National Transgender Health Summit, Oakland, CA, May. http://www.slideshare.net/kelleywinters/201305-nth-sb
Winter,S., Chalungsooth,P., Teh Y.K., Rojanalert,N., Maneerat, K., Wong Y.W., Beaumont, A., Ho, M.W., L., Gomez, F., and Macapagal, R.A. (2009). Transpeople, transprejudice and pathologisation: a seven-country factor analytic study. International Journal of Sexual Health, 21, 2: 96-118.
WPATH (2011). Standards of care for the health of transsexual, transgender, and gender nonconforming people (seventh version). WPATH. http://www.wpath.org